Abstract
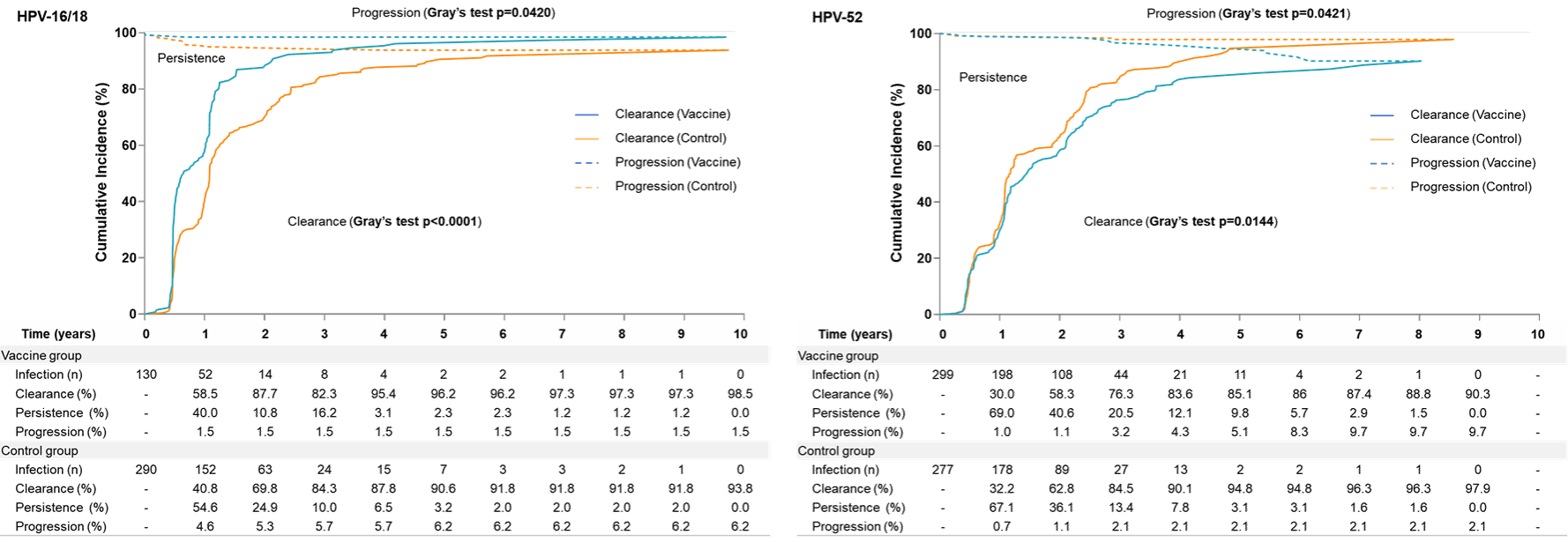
Existing evidence regarding the impact of vaccination on the natural history of high-risk human papillomavirus (HPV) infections remains limited, understanding such effects is essential for optimizing cervical cancer screening in post-vaccination era. Using 10-year follow-up data from a phase 3 randomized trial of the Escherichia coli-produced HPV-16/18 bivalent vaccine (NCT01735006) and its extension study (NCT05045755, NCT04969445), we compared the spectra and natural history (persistence, clearance, and progression) of high-risk HPV infections between vaccinated and unvaccinated females aged 18-45 years. Data was analyzed using the Cox regression and the competing risk model. Our findings indicate that vaccination reduces the burden of HPV-16/18-associated lesions (HR = 0.12, p = 0.0041) primarily by preventing incident infections (HR = 0.45, p < 0.0001) and modifying the natural history of breakthrough infections (enhancing clearance: 98.5% vs. 93.8%, p < 0.0001; and attenuating progression: 1.5% vs. 6.2%, p = 0.0420). Conversely, the elevated burden of HPV-52-associated lesions (HR = 3.06, p = 0.0303) observed in the vaccine group stems mainly from altered natural history (reduced clearance: 90.3% vs. 97.9%, p = 0.0144; and increased progression: 9.7% vs. 2.1%, p = 0.0421), rather than an increase in incidence (HR = 1.09, p = 0.2669). In this work, the observed shifts in HPV infection profiles and natural history between vaccinated and unvaccinated populations suggest that cervical cancer screening recommendations may warrant adjustment for vaccinated individuals.
Link:https://www.nature.com/articles/s41467-026-68379-3